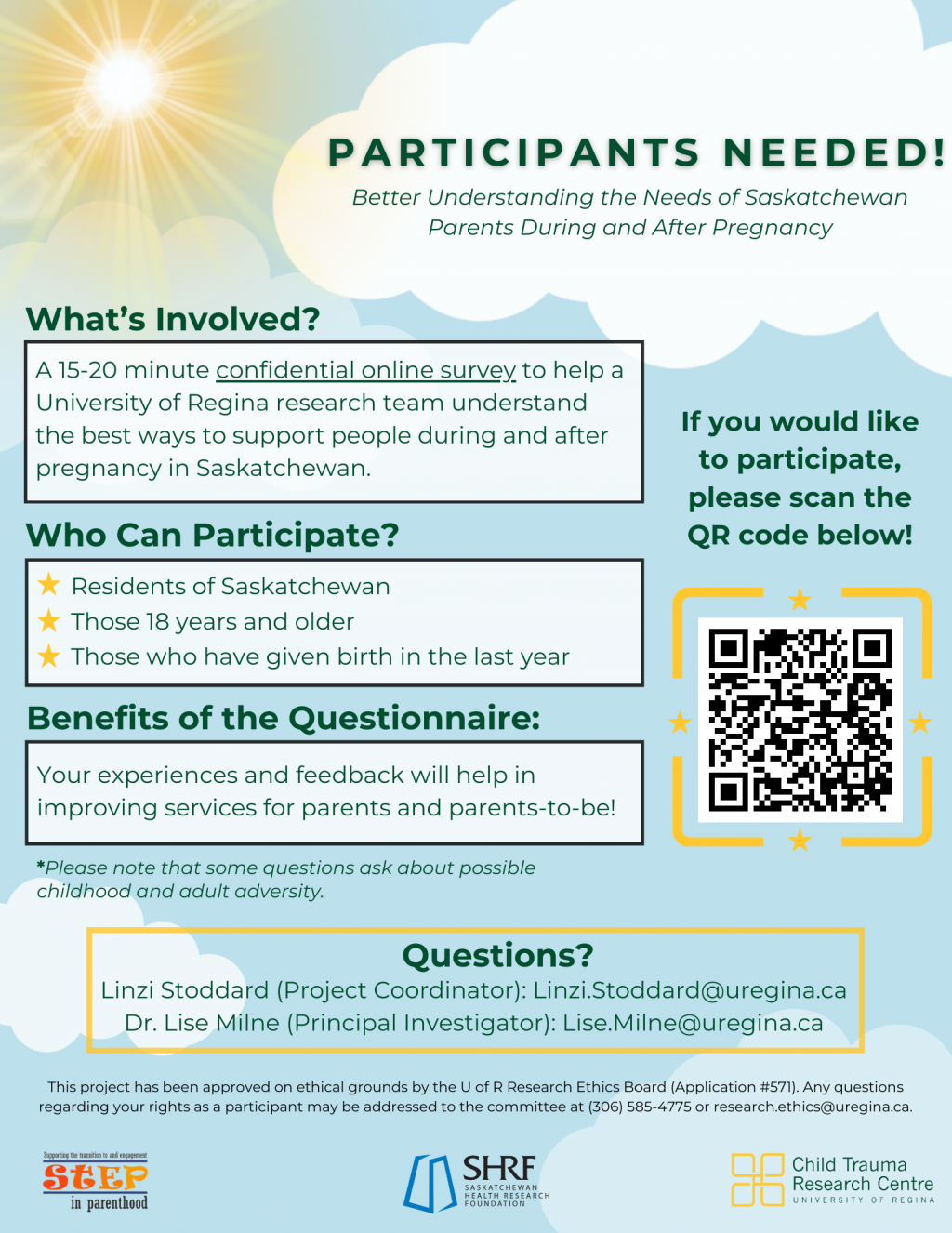
As part of a larger project aimed at supporting expectant parents, we are conducting a survey to better understand the support needs of Saskatchewan parents during and after pregnancy.
We want to hear from recent parents on their experiences in regards to perinatal services and programs in Saskatchewan. Some questions touch on potential adversity in childhood and adulthood, but having these experiences is not necessary to participate in the survey.
Who can participate?
Residents of Saskatchewan
Those 18 years and older
Those who have given birth in the last year
Would you like to share your thoughts and experiences with us? Please follow this link to an anonymous survey, which should take 15-20 minutes to complete. https://uregina.eu.qualtrics.com/jfe/form/SV_3dSJXGHrmDjG3SS
Your experiences and feedback will help in improving services for new parents and parents-to-be
This website is for educational purposes. If the situation is urgent, please call 911, or your local emergency services providers.